
Introduction to Certified Anesthesiologist Assistants (CAAs)
Certified Anesthesiologist Assistants (CAAs) are highly trained healthcare professionals who play a vital role in the field of anesthesia. With a specialized focus on patient safety and care, CAAs work collaboratively with anesthesiologists to provide top-notch perioperative care.
The demand for CAAs is on the rise, driven by the increasing complexity of medical procedures and the growing need for specialized anesthesia services. As healthcare continues to evolve, the role of CAAs becomes even more critical in addressing the diverse needs of patients and the healthcare system. Their specialized knowledge and skills make them a valuable asset in various clinical settings, including hospitals, outpatient surgical centers, and pain management clinics.
As the demand for skilled anesthesia providers grows, CAAs will continue to play a pivotal role in enhancing patient outcomes and advancing the field of anesthesiology.
States Where CAAs Are Licensed to Practice
Certified Anesthesiologist Assistants (CAAs) are recognized and licensed to practice in several states across the United States. Each state has specific licensing requirements and is regulated by different medical boards or state authorities, ensuring that CAAs meet the necessary qualifications to provide high-quality anesthetic care.
There are two types of state regulations: State Delegated authority and Licensure
Delegated authority means that a board certified Anesthesiologist can delegate tasks or duties related to the practice of anesthesiology to qualified CAAs. The physician remains ultimately responsible to the patient and the CAA must be qualified to be able to do the tasks.
Licensure of CAAs in the state means that there has been legislation enacted and codified into state law. Licensure would be the ultimate goal for CAAs as it firmly establishes CAAs in that state.
A more in-depth description can be found on the American Society of Anesthesiologist website: https://www.asahq.org/standards-and-practice-parameters/statement-on-certified-anesthesiologist-assistants-description-and-practice
Here is a comprehensive list of states where CAAs are licensed to practice, along with the relevant regulatory bodies and any state-specific variations in the scope of practice: https://www.anesthetist.org/about-caas
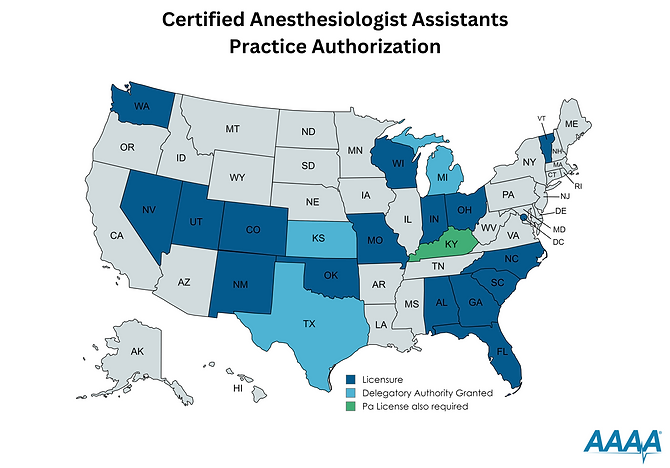
This image was obtained from the American Academy of Anesthesiologist Assistants website.
Alabama: The Alabama Board of Medical Examiners oversees the licensing of CAAs. In Alabama, CAAs must obtain certification from the National Commission for Certification of Anesthesiologist Assistants (NCCAA) and adhere to continuing education requirements.
Colorado: The Colorado Medical Board regulates CAAs. The state mandates completion of an accredited CAA program and passing the NCCAA exam.
District of Columbia: Licensure
Florida: Licensed by the Florida Board of Medicine, CAAs in Florida must meet strict certification and recertification standards. Additionally, they are required to work under the supervision of a licensed anesthesiologist.
Georgia: The Composite State Board of Medical Examiners in Georgia regulates CAAs. CAAs must be certified by the NCCAA and work in a team-based environment with anesthesiologists.
Guam: Delegatory authority
Indiana: The Indiana Medical Licensing Board requires CAAs to be certified and to operate under an anesthesiologist’s supervision.
Kansas: Delegatory authority
Kentucky: CAAs in Kentucky are licensed by the Kentucky Board of Medical Licensure, requiring NCCAA certification and adherence to state practice standards.
Michigan: Delegatory authority
Missouri: The Missouri Board of Registration for the Healing Arts oversees CAA licensing, requiring national certification and supervision by licensed anesthesiologists.
Nevada: Licensure
New Mexico: The New Mexico Medical Board licenses CAAs, who must be NCCAA-certified and meet state-specific regulations regarding practice and supervision.
North Carolina: The North Carolina Medical Board mandates that CAAs meet national certification requirements and state-specific guidelines for practice.
Ohio: The State Medical Board of Ohio licenses CAAs, necessitating NCCAA certification and defining a collaborative practice environment.
Oklahoma: The Oklahoma State Board of Medical Licensure and Supervision regulates CAAs, requiring certification and adherence to state practice standards.
Pennsylvania: Delegatory authority
South Carolina: CAAs are licensed by the South Carolina Board of Medical Examiners, requiring national certification and supervision by anesthesiologists.
Texas: The Texas Medical Board oversees the licensing of CAAs, mandating certification and supervision protocols.
Utah: 2022 Licensure
Vermont: The Vermont Board of Medical Practice licenses CAAs, requiring certification and adherence to state-specific guidelines for practice.
Washington: Licensure
Wisconsin: The Wisconsin Medical Examining Board regulates CAAs, necessitating certification and compliance with state practice regulations.
These states and territory not only recognize the essential role of CAAs in healthcare but also ensure that their practice is regulated to maintain the highest standards of patient care and safety. Prospective CAAs should consult with the respective state medical boards for detailed licensing procedures and requirements.
Outlook for more states
In the evolving landscape of healthcare, several states are currently considering legislation to permit Certified Anesthesiologist Assistants (CAAs) to practice within their borders. These legislative efforts are driven by a combination of advocacy from professional organizations and the pressing need to address healthcare workforce shortages.
Many AAs live in a state that they cannot work in and commute into a state that has licensure or delegatory authority on a daily basis.
States like Virginia, Maryland, New York have recently introduced bills aimed at integrating CAAs into their healthcare systems. Professional organizations, such as the American Academy of Anesthesiologist Assistants (AAAA), have been at the forefront of these advocacy efforts, providing critical data and engaging with lawmakers to underscore the benefits of CAAs. Each state has their own academy aimed at bringing CAA exposure to the state board of medicine. https://www.anesthetist.org/state-academies
The legislative process for allowing CAAs to practice typically involves several stages. Initially, a bill is proposed and must pass through various committees before it reaches the floor for debate. During this period, there is often significant lobbying by both proponents and opponents of the bill. Advocacy work by professional organizations can play a pivotal role in educating legislators about the role and qualifications of CAAs. Subsequently, the bill must be passed by both legislative chambers and signed into law by the governor.
The timeline for this process can vary greatly, ranging from several months to multiple years, depending on the state’s legislative calendar and the complexity of the bill. Not only is the state schedule important, but the question of will there be enough work to support both CAAs and CRNAs? After all, AA programs need to partner with local hospitals and institutions in order to be able to allow student AAs to undergo clinical training.
The potential impact of these legislative changes on healthcare systems is substantial. By expanding the workforce of skilled anesthesia providers, states can enhance the quality of care delivered to patients and reduce wait times for surgical procedures. Moreover, integrating CAAs into healthcare teams can alleviate the burden on anesthesiologists, allowing for more efficient use of medical resources and improving overall healthcare delivery.
Challenges and Opportunities in Expanding CAA Practice
The journey toward broader licensure for Certified Anesthesiologist Assistants (CAAs) is fraught with challenges, many of which stem from entrenched regulatory frameworks and resistance from other medical professionals. One of the primary barriers is the stringent state-by-state licensure requirements, which vary significantly and can often be an arduous process for CAAs to navigate. According to experts, this regulatory inconsistency can impede the mobility of CAAs, making it difficult for them to practice across state lines and limiting their professional opportunities.
Moreover, there is notable opposition from some sectors of the medical community, particularly among anesthesiologists and nurse anesthetists who may view the expansion of CAA practice as a threat to their own professional roles. This resistance is often based on concerns about maintaining high standards of patient care and ensuring that only the most qualified individuals are administering anesthesia. Despite these concerns, studies have shown that CAAs, under the supervision of anesthesiologists, provide care that is comparable in quality to other anesthesia providers.
On the flip side, the expansion of CAA practice presents significant opportunities for the healthcare system. One of the most compelling arguments in favor of broadening CAA licensure is the potential for improved access to anesthesia care, particularly in underserved areas where there may be a shortage of anesthesiologists. By integrating CAAs into the healthcare workforce more seamlessly, hospitals and clinics can alleviate bottlenecks and reduce wait times for surgical procedures, thus enhancing overall patient outcomes.
Additionally, the increased utilization of CAAs can help address the looming anesthesiologist shortage, which is projected to grow in the coming years. Incorporating more CAAs into the healthcare delivery model can ease the workload of anesthesiologists, allowing them to focus on more complex cases and improving the efficiency of anesthesia care teams.
Case studies from states where CAA practice has already been expanded highlight the benefits of this approach. For example, in places like Ohio and Georgia, CAAs have been successfully integrated into the healthcare system, providing high-quality anesthesia care and contributing to better patient outcomes. Looking forward, the future outlook for the CAA profession appears promising, with a growing recognition of the value that these professionals bring to the healthcare landscape.
